Although wearable devices can automatically detect Parkinson’s disease symptoms and inform clinicians about the progression of disease, the machine learning algorithms must be trained with annotated data from clinical experts who can recognize symptoms, and at the same time collecting such data are costly.
Northwestern Memorial Hospital in Chicago, IL conducted a study to investigate how to efficiently collect wearable sensor data for detection of bradykinesia and tremor in the upper extremities in people with Parkinson’s disease.
The study took place at Northwestern Memorial Hospital (Chicago, IL, USA) and was approved by the Northwestern University Institutional Review Board.
The results of the study were published in the journal Nature.
Parkinson’s disease (PD) is a long-term degenerative disorder of the central nervous system that mainly affects the motor system. It affects around 1% of people above 60 years of age in industrialized countries.
Read more Study Explores Use of Wearable Technology and Machine Learning to Monitor Parkinson’s Disease
Symptoms of Parkinson’s disease are: Tremor, Slowed movement (bradykinesia), Rigid muscles, Impaired posture, Loss of automatic movements, Speech changes and Writing changes.
The current gold standard of care to evaluate PD symptoms is through clinical examinations, whereby a trained clinician asks the patient to perform a series of standardized motor tasks (e.g. hand pronation-supination or heel tapping) while visually evaluating the quality of their movements and providing a symptom score.
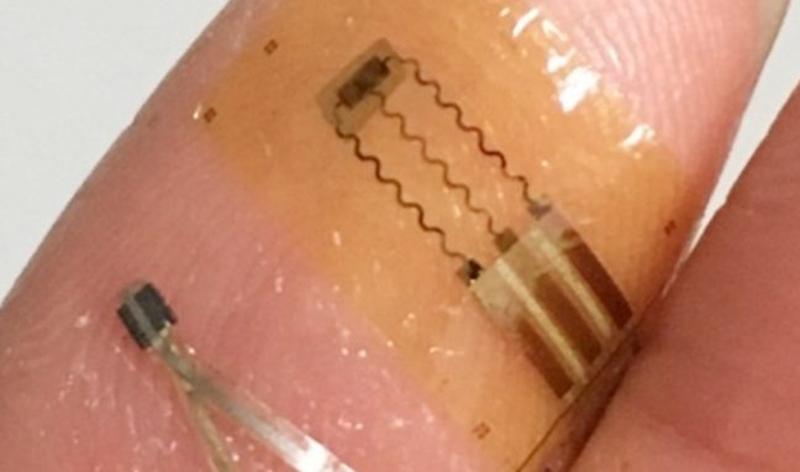
For their study, the researchers recruited 20 participants diagnosed with PD. Data from the participants were collected using soft wearable sensors, which adhere to the skin and are able to conform to its deformation during movements. This allows greater flexibility in sensor placement for collecting data from any part of the body, and with minimal burden for the wearer.
Results
The results showed that a single motion sensing device placed on the hand is sufficient to detect symptoms of tremor or bradykinesia in the upper extremities.
Combining data from sensors on both sides of the body did not aid detection on the impaired side, for bradykinesia and tremor. Other studies have evaluated the contribution of using non-movement sensing modalities, such as EMG, though it is unclear how necessary these modalities are for symptom detection.
The researchers also found that fine motor tasks and walking are suitable activities for automated evaluation of Parkinson’s Disease symptoms in the upper limbs using a single-hand sensor. Detection of bradykinesia and tremor from fine motor tasks or walking had comparable accuracy to detection from tasks used for clinical evaluation of these symptoms (e.g. finger to nose movements). Other studies have shown that motor symptoms can be quantified by prompting users to perform gait and finger tapping tests at home. The results suggest that fine motor tasks and walking may also be useful targets for symptom monitoring during naturalistic behaviors at home, according to the research team.
Limitations of the Study
Because of the limited number of individuals in this study who exhibited symptoms of dyskinesia, this study did not examine models for dyskinesia detection. Another limitation of the study was the fact that the team only had one rater for scoring the standardized motor assessments. Therefore, the researchers could not estimate the inter-rater variability, and thus the uncertainty of the target scores provided to the model.